What's Next For RF In Medicine?
By Ed Biller
Radio frequency and microwave technology often are thought of solely as communications tools, but their medical applications continue to expand.
Before looking at where we’re headed, though, let’s look at some of the staples that have defined RF use in medtech. The technology has been applied to surgery, imaging, and inter-device communications, to name just a few applications.
RF ablation technology uses RF energy to destroy unwanted tissues through a minimally invasive procedure. It can be used to eradicate cells with abnormal electrical activity — preventing arrhythmia (irregular heartbeat) — when delivered via a catheter, or to address tumor growth. Ablated tissue is replaced by healthy tissue through the body’s natural healing process.
In RF neurotomy/rhizotomy, generally used to treat back or neck pain, heat generated by radio waves targets specific nerves and temporarily interferes with their ability to transmit pain signals. This therapy can be used in addition to, or in lieu of, physical therapy and pharmaceuticals.
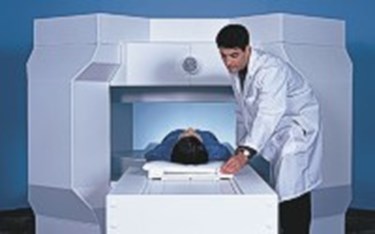
Magnetic resonance imaging (MRI) images the body’s anatomy (primarily water and fat) and physiological processes using strong magnetic fields, radio waves, and electrical field gradients.
Of course, communication still forms the backbone of RF technology’s utility in medicine. From pacemakers and subcutaneous implantable defibrillators (S-ICDs) that communicate with one another inside the body, to the practice of telemedicine in rural areas of large nations, leveraging RF technology to transmit/receive information continues to make its mark in medtech.
So, what’s next?
Unsurprisingly, as the Internet of Things permeates consumer devices, medtech has been on the leading edge of the trend. Connected medical devices make telemedicine feasible and effective, empower caregivers and allow patients to take a more active role in their care, and reduce healthcare ecosystem costs by minimizing doctor visits (often by transmitting data gathered by “smart” monitoring devices directly to doctors).
This trend runs the gamut of medical devices, many of which are aimed at home use. The world’s first Bluetooth-connected insulin pen launched in Europe this month and is expected to receive FDA approval in the U.S. later this year, and a Bluetooth-enabled, touchless thermometer launched in the U.S. earlier this summer.
Other initiatives are reevaluating how RF is used in established medical technologies. For example, in 2013, researchers at Case Western Reserve University found a way to speed MRI’s imaging process by overlapping signals to create a magnetic resonance “fingerprint” (MRF) matched to tissue qualities. Then, this summer, researchers at NYU Langone Medical Center designed "Plug-and-Play MR Fingerprinting" (PnP-MRF). This innovation is a circling strobe light of many broadcast magnetic fields, versus MRF’s single-source radio wave pulses; it creates layers of images by pulsing radio waves separated by a few milliseconds. Dark spots present in one image may not be visible in the next, allowing for more complete images and paving the way toward table-top or even hand-held MRI devices, according to the researchers.
Also, traditional marking of cancerous breast lesions for removal involves the injection of radioactive materials or wire localization — wherein surgeons are directed by a wire that protrudes from the patient’s breast. But one company’s implantable “reflector,” available in the U.S. as of late last year, offers another option: radar localization. Studies suggest the method both is clinically effective and improves patient experience.
Even elective procedures are getting in on the action: Despite the devices’ technical limitations, RFID chip implants offer a number of intriguing options. They have proven capable of navigating the FDA approval process, having (briefly) been leveraged to verify identity and medical history. One day, RFID implants may again fill that role, providing medical professionals with vital medical history information on-the-spot. But first, misinformation like the notion of governments tracking citizens through their RFID chips has to be dispelled from the public consciousness.
More realistic RFID implant applications include an Ohio implant company’s initiative to monitor strain on its spinal fusion rods using RFID technology. Numerous tissue-integrated health monitoring devices also are in development, many of which use RFID technology to communicate with a smartphone app, allowing users to track key biomarkers in real time.
The bottom line is, design engineers are stretching their wings as they look at unmet therapeutic needs. Even with the hurdles of FDA regulation, cybersecurity concerns, and the labyrinthine world of spectrum allocation, there is so much RF-related innovation in medtech right now, it’s difficult to pick and choose what to mention here.
Did I miss anything groundbreaking, or even just interesting? What applications should medtech be exploring? I look forward to continuing the discussion in the Comments section below.
(EDITOR NOTE: Since this article was penned, engineers at the University of Washington have discussed some of their research using "interscatter" communications to help low-power medical implants communicate outside the body.)
